6. Detection and Management of Modifiable Risk Factors
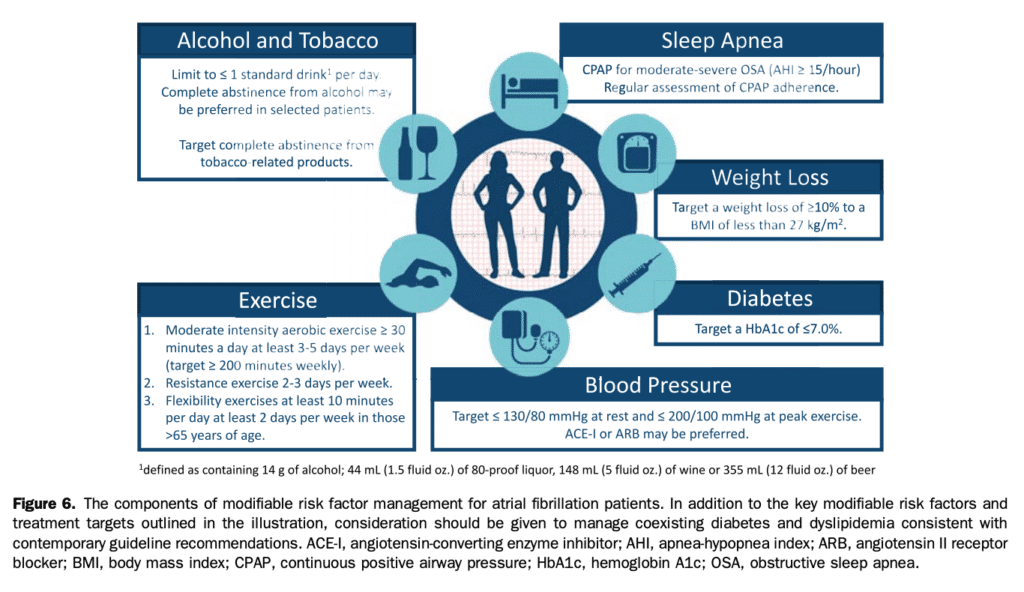
Modifiable cardiovascular risk factors are well recognized contributors to the development and progression of AF.[29],[65],[66] These established, emerging, and potential risk factors for AF have been summarized in section 3, and Tables 1 and 2. The risk of developing AF increases with the severity and number of modifiable cardiovascular risk factors (such as hypertension, diabetes mellitus, and obesity). In many cases this risk increase is linear within and between risk factors and might be apparent even within the established “normal range.” For example, a systolic BP in the prehypertensive range (130-139 mm Hg) has been associated with a 28% higher adjusted risk of developing AF compared with a systolic BP < 120 mm Hg.[119] Similarly, although the corrected AF incidence increases approximately 5% for each unit increase in body mass index (BMI),[120] weight gain has been associated with incident AF independent of BMI (34% increased AF with a 16%-35% weight gain, and 61% increased AF with a > 35% weight gain).[121] In light of the breadth of data supporting an association between these modifiable cardiovascular risk factors and AF incidence, it has been suggested that the implementation of lifestyle modification and risk factor intervention could significantly decrease the incidence of AF. Unfortunately, the evidence to support targeted risk factor modification to prevent incident AF is limited, in part because of the observation that the absolute risk increase of incident AF from any individual risk factor is low. As such, two complementary approaches have been proposed. The first is to target preventive intervention in individuals who are at highest risk for AF occurrence. Identification of these individuals could be accomplished through the use of risk prediction models or, potentially, with artificial intelligence-enabled screening algorithms.[122]–[124] When identified, these high-risk populations could be targeted for comprehensive risk factor modification. However, it is important to recognize that a focus on only those identified as at highest risk of developing AF would miss the opportunity to prevent most incident cases of AF because these occur in the large segment of the population typically considered to be at “lower risk.” As such, decreasing the population effect of AF will require broad implementation of lifestyle modification strategies (eg, a focus on physical activity, and avoidance of alcohol and tobacco consumption) in addition to targeted intervention of traditional cardiovascular risk factors (including hypertension, HF, diabetes, OSA, and obesity) in those at highest risk of AF development. In patients with established AF, the relationship between risk factor intervention and AF outcomes is well recognized. Several studies have shown that continuous positive airway pressure usage in patients with OSA is associated with a lower risk of AF recurrence compared with nonusage, with rates of recurrent AF comparable with those in patients without OSA.[125]–[127] Many studies have shown that targeted weight loss interventions significantly reduce AF burden (number and cumulative duration of AF episodes)and AF symptom severity scores.[128]–[130] The Long-Term Effect of Goal-Directed Weight Management on Atrial Fibrillation Cohort: A Long-Term Follow-Up Study (LEGACY) cohort study showed that patients with a weight loss of > 10% was associated with a sixfold increase in the likelihood of being arrhythmia-free over a 5-year follow-up compared with those with lesser degrees of weight loss.[129] Abed et al. showed that weight reduction with intensive risk factor management resulted in a significant improvement in AF-related QOL, AF symptom scores, and AF burden.[128] The Impact of Cardiorespiratory Fitness on Arrhythmia Recurrence in Obese Individuals with Atrial Fibrillation (CARDIO-FIT) study showed that a > 2 Metabolic Equivalents (METs) improvement in cardiorespiratory fitness was associated with a significantly reduced AF burden compared with a gain of < 2 METs over longterm follow-up.[131] AF burden reduction was proportional to the increase in cardiorespiratory fitness, with an adjusted reduction in AF recurrence of 10% for each MET gained (hazard ratio [HR], 0.90; 95% CI, 0.83-1.00).[131] Rienstra et al. showed improved maintenance of sinus rhythm at 1 year with a strategy of cardiac rehabilitation, HF medication optimization, and aggressive BP control (75% maintenance of sinus rhythm on a 7-day Holter vs 63% in the control group; OR, 1.77, P ¼ 0.042).[132] The Aggressive Risk Factor Reduction Study for Atrial Fibrillation and Implications for the Outcome of Ablation (ARREST-AF) single-centre cohort study showed that patients who chose to undergo aggressive risk factor modification had better QOL and symptom control, a significant reduction in AF burden, and greater arrhythmia-free survival after catheter ablation compared with those who did not (OR, 4.8; 95% CI, 2.04-11.4; P < 0.001).[65] Taken together, these data suggest that outcomes might be improved by using a comprehensive management strategy that includes suppression of triggers (targeted by risk factor modification, antiarrhythmic drugs, and/or catheter ablation) and amelioration of arrhythmogenic substrate (risk factor modification). Treatment targets for modifiable risk factor intervention are presented in Figure 6.
Recommendation
11. In patients with established AF or at high risk of developing AF, we recommend a systematic approach to the identification of traditional modifiable cardiovascular risk factors and/or conditions associated with AF, with strict guideline-adherent management to reduce major cardiovascular events (Strong Recommendation; High-Quality Evidence) and to prevent recurrence of the arrhythmia and/or decrease its symptom burden (Strong Recommendation; Low-Quality Evidence).
Values and Preferences
This recommendation places a high value on a comprehensive, holistic, and systematic approach to the management of AF. Because of the contribution of modifiable risk factors to the development and progression of AF, a systematic approach to the identification of modifiable cardiovascular risk conditions offers a potential therapeutic target to improve outcomes in this population. This recommendation recognizes the association between these modifiable cardiovascular risk factors (including but not limited to hypertension, HF, diabetes mellitus, obesity, inactivity, sleep apnea, and alcohol misuse), and major adverse cardiovascular outcomes (eg, stroke, MI, cardiovascular death) and AF outcomes (AF burden/exacerbations, AF-related ED visits/hospitalizations).
Practical Tip
Screening for common cardiovascular risk factors and/or conditions (hypertension, obesity, inactivity, sleep apnea, diabetes, and alcohol misuse) should be performed in addition to screening for AF-specific risk conditions (HF, valvular heart disease, thyroid dysfunction).
References
29. Andrade J, Khairy P, Dobrev D, Nattel S. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res 2014;114:1453-68.
65. Pathak RK, Middeldorp ME, Lau DH, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol 2014;64:2222-31.
66. Lau DH, Nattel S, Kalman JM, Sanders P. Modifiable risk factors and atrial fibrillation. Circulation 2017;136:583-96.
119. Mitchell GF, Vasan RS, Keyes MJ, et al. Pulse pressure and risk of newonset atrial fibrillation. JAMA 2007;297:709-15.
120. Dublin S, French B, Glazer NL, et al. Risk of new-onset atrial fibrillation in relation to body mass index. Arch Intern Med 2006;166:2322-8.
121. Rosengren A, Hauptman PJ, Lappas G, et al. Big men and atrial fibrillation: effects of body size and weight gain on risk of atrial fibrillation in men. Eur Heart J 2009;30:1113-20.
122. Schnabel RB, Sullivan LM, Levy D, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet 2009;373:739-45.
123. Alonso A, Krijthe BP, Aspelund T, et al. Simple risk model predicts incidence of atrial fibrillation in a racially and geographically diverse population: the CHARGE-AF consortium. J Am Heart Assoc 2013;2:e000102.
124. Attia ZI, Noseworthy PA, Lopez-Jimenez F, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet 2019;394:861-7.
125. Fein AS, Shvilkin A, Shah D, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol 2013;62:300-5.
126. Li L, Wang ZW, Li J, et al. Efficacy of catheter ablation of atrial fibrillation in patients with obstructive sleep apnoea with and without continuous positive airway pressure treatment: a meta-analysis of observational studies. Europace 2014;16:1309-14.
127. Shukla A, Aizer A, Holmes D, et al. Effect of obstructive sleep apnea treatment on atrial fibrillation recurrence: a meta-analysis. JACC: Clin Electrophysiol 2015;1:41-51.
128. Abed HS, Wittert GA, Leong DP, et al. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA 2013;310:2050-60.
129. Pathak RK, Middeldorp ME, Meredith M, et al. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a longterm follow-up study (LEGACY). J Am Coll Cardiol 2015;65:2159-69.
130. Mahajan R, Lau DH, Brooks AG, et al. Electrophysiological, electroanatomical, and structural remodeling of the atria as consequences of sustained obesity. J Am Coll Cardiol 2015;66:1-11.
131. Pathak RK, Elliott A, Middeldorp ME, et al. Impact of CARDIOrespiratory FITness on arrhythmia recurrence in obese individuals with atrial fibrillation: the CARDIO-FIT study. J Am Coll Cardiol 2015;66:985-96.
132. Rienstra M, Hobbelt AH, Alings M, et al. Targeted therapy of underlying conditions improves sinus rhythm maintenance in patients with persistent atrial fibrillation: results of the RACE 3 trial. Eur Heart J 2018;39:2987-96.
