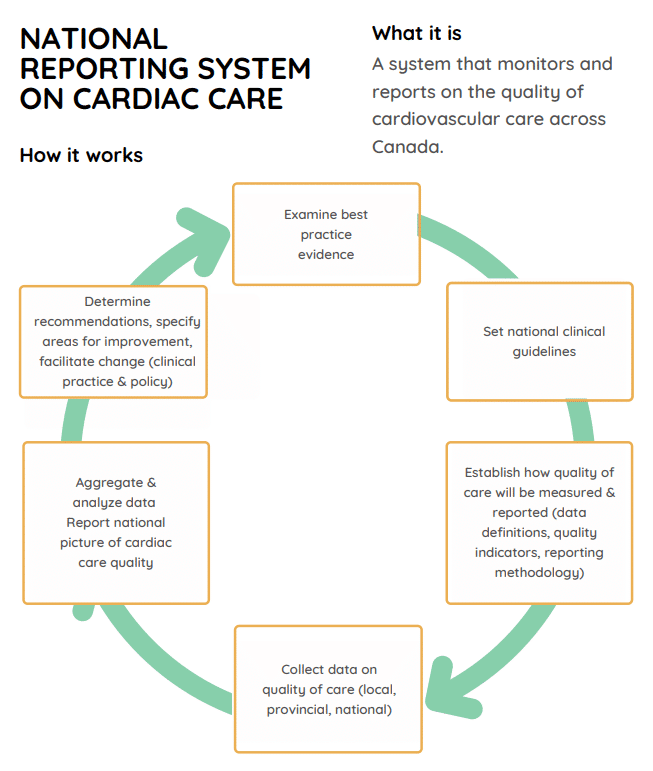
Quality Reporting
The CCS supports and advocates for measuring and reporting national cardiovascular care quality to:
- Make regional comparisons that highlight where changes are needed;
- Make evidence-based improvements that close gaps in care; and
- Ensure accountability for efficient use of resources and optimal health system performance.
Evidence suggests that:
Since 2017, the CCS has called on the federal government to invest in national quality reporting through several pre-budget submissions & testimonies before the federal Finance Committee.
Watch Dr. Andrew Krahn’s appearance before the Federal Standing Committee on Finance (February 2020).
Read our federal pre-budget submissions: 2017, 2018, 2019, 2020.
Dr. Andrew Krahn’s appearance before the Federal Standing Committee on Finance
Quality reporting resources
Through national consultation, the CCS established how cardiovascular care quality is defined and measured. We encourage local, regional, and national stakeholders to use these resources to inform and facilitate consistent measurement and reporting of care quality across Canada.
- Data definitions: defines how care quality is measured. The Core Elements and Demographics data definitions includes guidelines for data elements and definitions related to demographics, history and risk factors, co-morbidities, test results, symptoms, and medications. This is supplemented with six chapters organized by specific areas of care.
- Quality indicators: designed to assess quality based on structures (e.g., wait time), processes (e.g., length of stay), and outcomes (e.g., 30-day mortality) and developed using best practice methodology.
- Risk adjustment models: refers to statistical models to account for differences in demographic and clinical characteristics of patients to allow comparison of hospital outcomes.
Data definitions and quality indicators have been developed for the following cardiovascular care areas:
| Atrial Fibrillation/Flutter | data definitions | quality indicators | |
| Coronary Artery Disease / Acute Coronary Syndrome – Cardiac Surgery – Percutaneous Coronary Intervention (PCI) – Transcatheter Aortic Valve Implantation (TAVI) | data definitions data definitions | quality indicators quality indicators quality indicators | risk adjustment model |
| Cardiac Rehabilitation | data definitions & quality indicators | ||
| Heart Failure | data definitions | quality indicators |
CCS national quality reports
The CCS has produced the following national reports on cardiovascular care quality:
- Cardiac Care Quality Indicators (CCQI) report in partnership with the Canadian Institute for Health Information (CIHI). The final 2022 update includes data on mortality rates following percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG), aortic valve replacement (AVR), and combined AVR and CABG, as well as readmission rates after PCI and isolated CABG.
Review previous reports and updates from 2020, 2019, 2018 and 2017.
Review the 2019 Cardiac Surgery and PCI commentaries.
- “The State of Heart Failure Care in Canada: Minimal Improvements in Readmissions Over Time Despite and Increased Number of Evidence-based Therapies” reveals the 30-day readmission rate for heart failure (HF) patients has not changed in the last decade.
- The 2019 National Quality Report: TAVI provides an updated pan-Canadian snapshot of TAVI care across the country between 2013 and 2017.
You can also view the 2016 National Quality Report: TAVI.
- Fonarow GC. Improving quality of care and outcomes for heart failure–role of registries. Circ J. 2011. 1106291286-1106291286.
- Ambrosy AP, Fonarow, GC, Butler J et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123-33.
- Young C, Lambert L, Abel J et al. Quality of cardiac care in Canada: recommendations for building a sustainable future. Can J Cardiol. 2018;34:800-03.
- Tyrrell L. The impacts of public reporting and external benchmarking in cardiac care: a rapid update of the literature. Institute of Health Economics. 2017.